Back
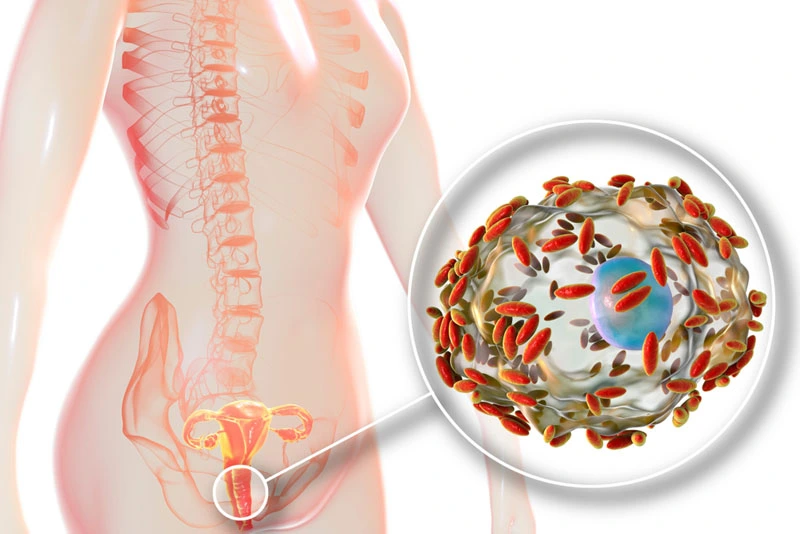
Bacterial vaginosis (BV) vs Urinary Tract Infection (UTI)
By Shannon Strauch, PTA, STMT-1 on 5/9/2024
Bacterial vaginosis (BV) and urinary tract infections (UTIs) are two different conditions that affect the genital and urinary systems, respectively. Here are some key differences between the two:
Location of Infection
:BV primarily affects the vagina and is characterized by an imbalance of bacteria, where harmful bacteria outnumber beneficial ones.
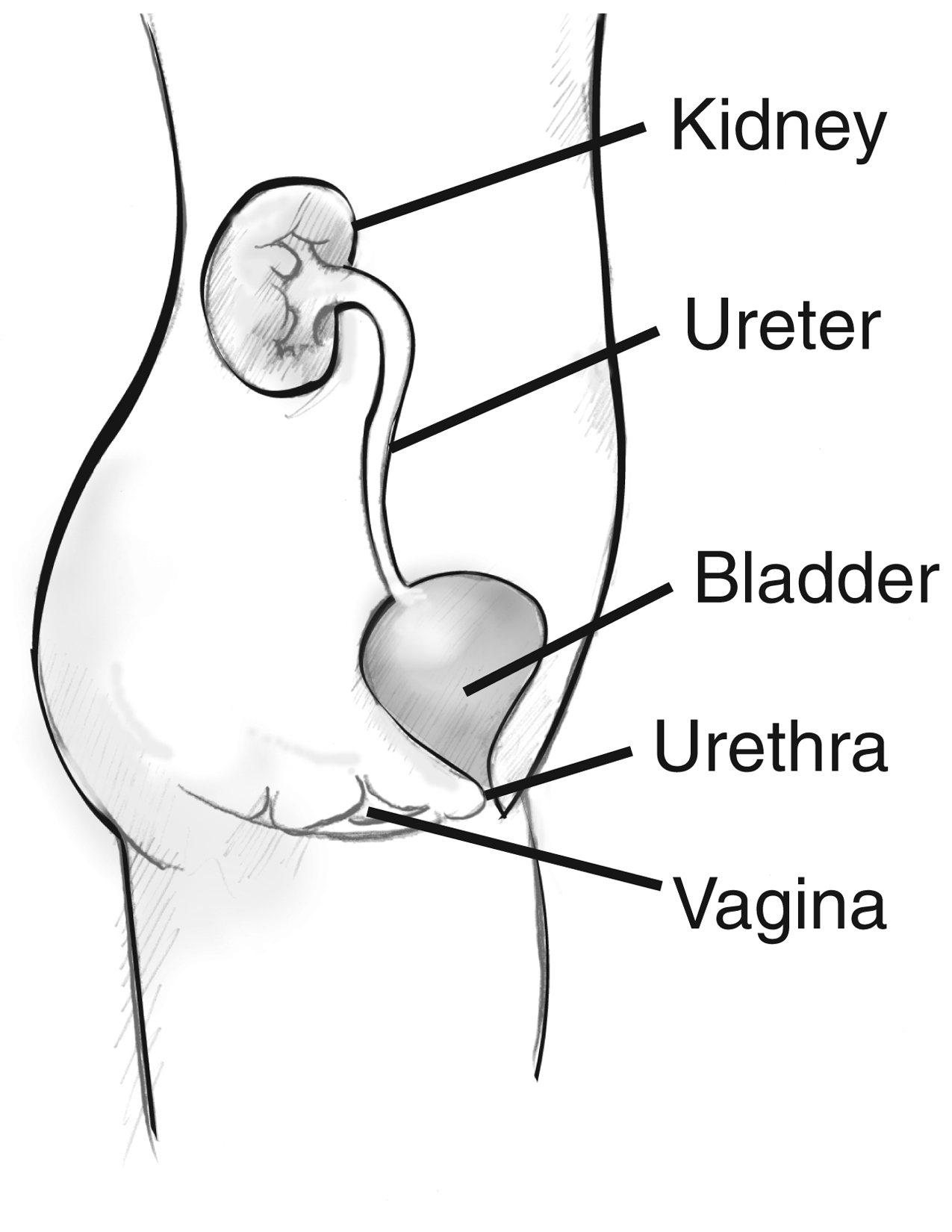
UTIs, on the other hand, occur in the urinary tract, which includes the bladder, urethra, ureters, and kidneys.
Symptoms
:BV symptoms often include a thin, grayish-white vaginal discharge with a fishy odor, along with itching or irritation in the vaginal area.
UTI symptoms typically include a strong, persistent urge to urinate, burning sensation during urination, cloudy or bloody urine, and pelvic pain.
Causes
:BV is often caused by an overgrowth of harmful bacteria like Gardnerella vaginalis, leading to a disruption of the normal vaginal flora.
UTIs are commonly caused by bacteria such as Escherichia coli (E. coli) that enter the urinary tract through the urethra and multiply, causing infection.
Risk Factors
:Risk factors for BV include sexual activity (especially with multiple partners), douching, and hormonal changes.
Risk factors for UTIs include female anatomy (shorter urethra), sexual activity, use of certain contraceptives (like diaphragms), menopause, and urinary tract abnormalities.
Diagnosis
:BV is diagnosed through a physical examination, evaluation of symptoms, and laboratory tests such as vaginal pH testing and microscopic examination of vaginal discharge.
UTIs are diagnosed through a urinalysis (testing urine for bacteria and white blood cells) and sometimes urine culture to identify the specific bacteria causing the infection.
Treatment
:BV is typically treated with antibiotics, such as metronidazole or clindamycin, to restore the balance of vaginal bacteria.
UTIs are also treated with antibiotics, targeting the specific bacteria causing the infection. Common antibiotics for UTIs include trimethoprim-sulfamethoxazole, nitrofurantoin, and ciprofloxacin.
It's essential to seek medical advice for accurate diagnosis and treatment of both BV and UTIs, as untreated infections can lead to complications or recurrence.
Pelvic floor therapy primarily focuses on the muscles, ligaments, and connective tissues in the pelvic region. While it may not directly treat bacterial vaginosis (BV) or urinary tract infections (UTIs), it can play a supportive role in managing these conditions and promoting overall pelvic health. Here's how pelvic floor therapy can help:
Pelvic Floor Muscle Strengthening
: Pelvic floor therapy includes exercises to strengthen the pelvic floor muscles. Strengthening these muscles can improve bladder and bowel control, reducing the risk of urinary incontinence and promoting better bladder health. This can be beneficial for individuals prone to UTIs or those experiencing pelvic floor dysfunction alongside BV or UTIs.Pelvic Floor Relaxation Techniques
: In cases where pelvic floor muscles are tight or overactive (a condition known as hypertonic pelvic floor dysfunction), pelvic floor therapy can teach relaxation techniques. Relaxing these muscles can help alleviate pelvic pain, discomfort, and urinary urgency, which are common symptoms associated with UTIs and BV.Education on Pelvic Health
: Pelvic floor therapy often involves education on pelvic health, including proper toileting techniques, hygiene practices, and lifestyle modifications. This education can help prevent recurrent UTIs by promoting healthy urinary habits and reducing the risk of bacterial contamination.Posture and Alignment
: Pelvic floor therapy may address posture and alignment issues that can contribute to pelvic floor dysfunction. Correcting posture can relieve pressure on the pelvic organs, improve circulation, and optimize pelvic floor function, indirectly benefiting individuals with BV or UTIs.Biofeedback and Electrical Stimulation
: Some pelvic floor therapy techniques involve biofeedback and electrical stimulation. Biofeedback helps individuals gain awareness and control over their pelvic floor muscles, which can be helpful in managing urinary symptoms. Electrical stimulation may also be used to strengthen or relax specific muscle groups as part of the therapy process.Comprehensive Treatment Approach
: Pelvic floor therapy is often part of a comprehensive treatment approach that may include medical interventions for BV or UTIs. By addressing pelvic floor dysfunction and promoting pelvic health, therapy can complement medical treatments and improve overall outcomes.
It's important to consult with a healthcare professional, such as a pelvic floor therapist or urologist, to determine the most appropriate treatment plan for BV, UTIs, and any associated pelvic floor issues. Individualized care and a holistic approach to pelvic health can lead to better management and prevention of these conditions.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment