Back
How Constipation Can Impact Pelvic Floor and Bladder Health
By Dr. Christine Martirez PT, DPT on 11/5/2024
Chronic constipation isn’t just uncomfortable—it can also disrupt the function of nearby pelvic organs, particularly the bladder. Understanding the interconnected anatomy of the pelvic organs helps shed light on why constipation affects bladder health and urinary function. For those struggling with chronic constipation, symptoms like urinary incontinence and decreased bowel movement sensation can be common associated symptoms. Pelvic floor therapy offers targeted techniques to address these issues, helping to improve bowel regularity, alleviate bladder symptoms, and support overall pelvic health.
Anatomy of the Pelvic Organs and Their Close Relationship
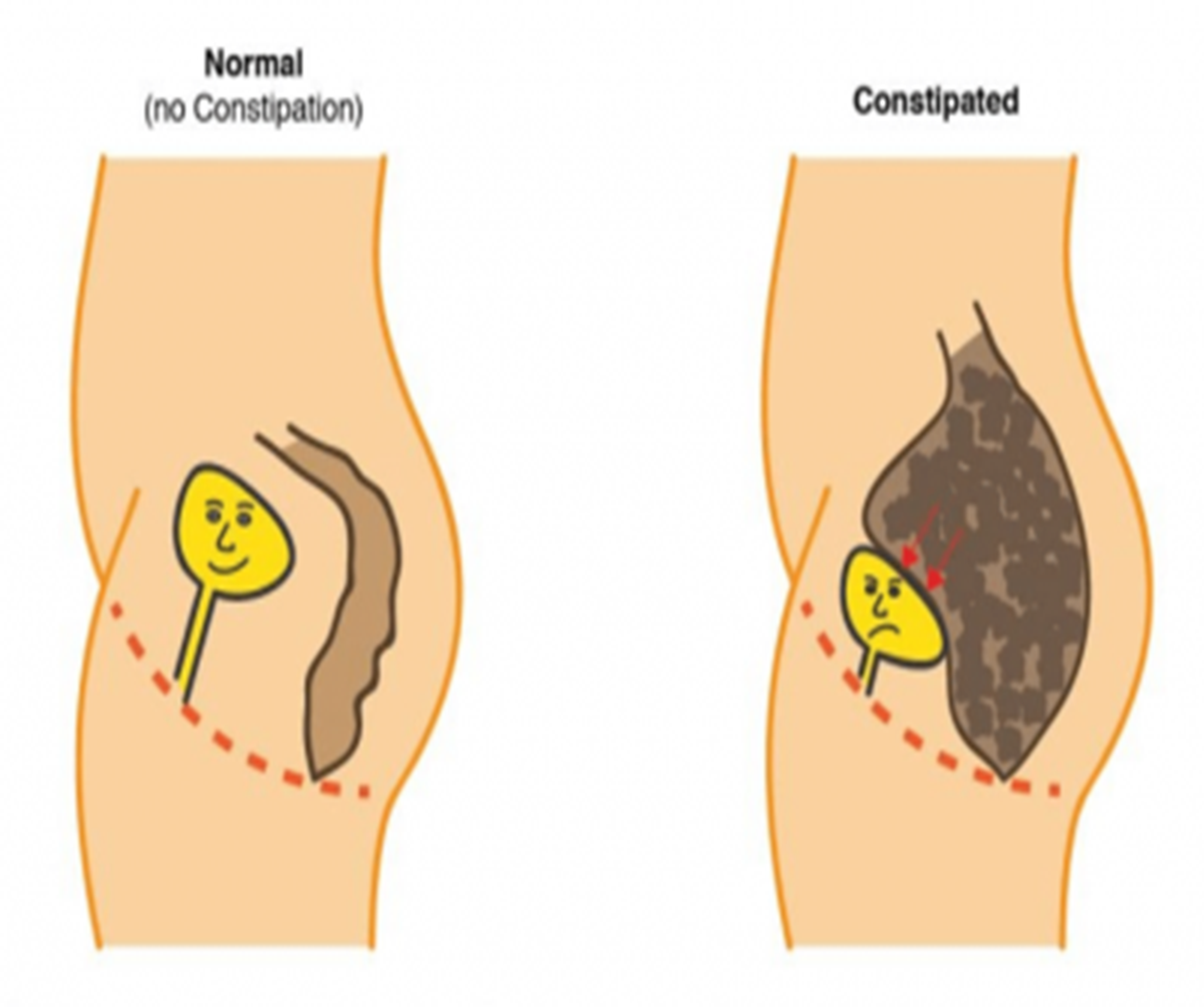
The pelvic organs share a small, confined space in the pelvis. For people with female anatomy, the bladder sits at the front of the pelvis, the uterus and vagina are located in the middle, and the rectum is positioned toward the back. For those with male anatomy, the bladder is positioned in front of the rectum, with the prostate gland lying just below the bladder, surrounding the urethra. Due to this close anatomical relationship, each organ’s function can significantly impact the others. When the rectum is impacted by constipation, it can press on surrounding organs, particularly the bladder. This pressure can lead to a variety of bladder and pelvic floor dysfunction symptoms, and in cases of severe or prolonged constipation, it may affect the sensation and function of the bladder.
How Chronic Constipation Affects Bladder and Pelvic Floor Function
Increased Pressure on the Bladder
Chronic constipation can cause stool buildup in the rectum, increasing pressure on the bladder and reducing its capacity to store urine comfortably. The bladder may feel fuller sooner, resulting in frequent urges to urinate. Additionally, the increased pressure can interfere with bladder emptying, leading to urinary retention and recurrent urinary tract infections (UTIs) as a result of incomplete emptying.Exacerbation of Urinary Incontinence
Pelvic floor muscles support the bladder, rectum, and other pelvic organs. When constipation is chronic, the pelvic floor muscles may become tight or fatigued from increased straining. This tension can impact the support structure for the bladder and urethra, exacerbating symptoms of urinary incontinence. Stress incontinence, for example, may worsen as the overactive or weakened pelvic floor struggles to control urinary leakage.Decreased Sensation for Bowel Movements
Over time, chronic constipation can dull the sensation for having a bowel movement. This decreased sensation can be due to prolonged stool retention, which overstretches the rectum and reduces the urge to defecate. This feedback loop—less urge, more constipation—can further strain the pelvic floor, making it difficult to develop a healthy bowel routine and leading to increased bladder symptoms as the rectal pressure on the bladder remains constant.Tension and Dysfunction in the Pelvic Floor Muscles
The pelvic floor muscles play a critical role in supporting the pelvic organs, maintaining continence, and helping with stool passage. Chronic constipation can create hypertonicity, or excessive muscle tension, in the pelvic floor as the muscles compensate for stool retention. This tension can lead to dysfunction and interfere with the relaxation required for effective bowel and bladder emptying. As a result, symptoms like urinary frequency, urgency, and incomplete emptying may worsen.
How Pelvic Floor Therapy Can Help with Constipation and Bladder Health
Pelvic floor physical therapy provides targeted treatment for the issues that arise from chronic constipation and its effects on the bladder and surrounding organs. Therapists focus on improving muscle coordination, enhancing pelvic floor relaxation, and creating strategies to support natural and healthy elimination.
Pelvic Floor Muscle Relaxation and Retraining
A key focus of pelvic floor therapy for those with constipation and bladder issues is to release excessive tension in the pelvic floor muscles. Manual therapy techniques help to relax and lengthen these muscles, reducing strain on the bladder and supporting normal bowel movements. Therapists also provide exercises to retrain the pelvic floor for balanced support without excessive tension.Biofeedback and Sensory Re-education
Biofeedback can help increase awareness of the pelvic floor muscles, teaching patients to properly relax these muscles during bowel and bladder functions. For those with decreased sensation due to chronic constipation, biofeedback can aid in retraining bowel and bladder awareness to restore normal sensation and timing for elimination.Education on Proper Toileting Posture and Techniques
Pelvic floor therapists teach proper toileting techniques to minimize strain, such as using a small stool to elevate the feet for an optimal rectal angle and practicing breathing techniques to ease stool passage. These techniques reduce stress on the pelvic floor and bladder, helping relieve constipation and urinary symptoms.Core and Diaphragmatic Breathing Exercises
Therapists work with patients to improve core stability and teach diaphragmatic breathing exercises that support proper abdominal pressure management. These exercises encourage effective bowel and bladder emptying while reducing strain, which ultimately supports pelvic floor health and minimizes bladder irritation.Establishing Healthy Bowel Routines and Dietary Recommendations
Pelvic floor therapists offer guidance on dietary choices to support regularity and may suggest lifestyle modifications to encourage daily bowel movements. Hydration and fiber intake are emphasized, along with recommendations on establishing a regular routine for healthy elimination habits.
Supporting Both Bowel and Bladder Health
Chronic constipation can create a range of urinary symptoms due to the close relationship between pelvic organs. By addressing the root causes of constipation and learning pelvic floor-friendly elimination techniques, patients can relieve their bladder symptoms and support overall pelvic health. Pelvic floor therapy empowers individuals to manage their pelvic floor muscles effectively, reduce tension and strain, and develop healthier toileting habits. In doing so, it offers a holistic approach that helps to break the constipation-bladder symptom cycle and restores balance and comfort to the pelvic floor.
Suffering from constipation and other pelvic floor related issues? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment