Back
How Do I Help My Child From Wetting the Bed?
By Shannon Strauch, PTA, STMT-1 on 5/24/2024
Pelvic floor therapy can be an effective approach to addressing bedwetting, also known as nocturnal enuresis, especially in children but sometimes in adults as well. Bedwetting can be a complex condition influenced by various factors, including bladder dysfunction, deep sleep patterns, hormonal factors, and psychological issues. Pelvic floor therapy aims to strengthen and coordinate the muscles of the pelvic floor, which play a crucial role in bladder control. Here’s how pelvic floor therapy can help with bedwetting:
Understanding Bedwetting
Bladder Control
:Bedwetting occurs when there is involuntary urination during sleep. This can be due to an overactive bladder, a small bladder capacity, or a delay in the maturation of the bladder control system.
Micturition Reflex:
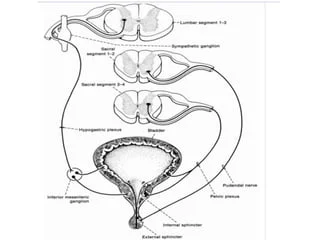
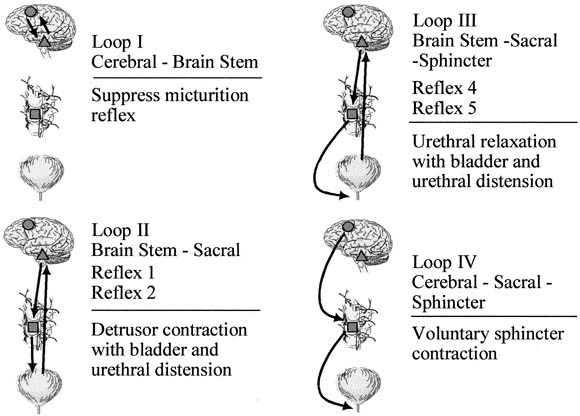
The micturition reflex is a pathway that allows for urination, or micturition. It's an autonomic reflex that involves the bladder contracting and the urethra relaxing simultaneously through the Bradley's Loops. The reflex is triggered when the bladder wall's stretch receptors are stimulated by the bladder collecting around 300–400 mL of urine. This creates sensory impulses that lead to urination.
Pelvic Floor Muscles
:The pelvic floor muscles support the bladder and help control the release of urine. Weak or poorly coordinated pelvic floor muscles or ligaments can contribute to bedwetting.
How Pelvic Floor Therapy Helps
Muscle Strengthening
:Strengthening the pelvic floor muscles can improve bladder control. Exercises such as Kegels, which involve contracting and relaxing the pelvic floor muscles, can enhance muscle strength and endurance.
Stronger muscles can better support the bladder and urethra, reducing the likelihood of involuntary urination.
Biofeedback Training
:Biofeedback is a technique used in pelvic floor therapy to help individuals become more aware of their pelvic floor muscles and how to control them.
Through visual or auditory feedback, patients learn to contract and relax their pelvic floor muscles properly, improving muscle coordination and bladder control.
Bladder Training
:Bladder training involves techniques to increase bladder capacity and improve the timing of urination. This can include scheduled voiding and gradually increasing the intervals between bathroom visits.
Combined with pelvic floor exercises, bladder training can help regulate the urge to urinate and reduce the frequency of bedwetting episodes.
Behavioral Interventions
:Pelvic floor therapists often incorporate behavioral interventions such as fluid management, reducing evening fluid intake, and establishing a regular bedtime routine.
These interventions can complement pelvic floor exercises and improve overall bladder control.
Addressing Underlying Conditions
:Pelvic floor therapy can help identify and address underlying conditions that may contribute to bedwetting, such as constipation, urinary tract infections, or pelvic floor dysfunction.
Treating these conditions can reduce the frequency and severity of bedwetting.
Special Considerations for Children
Age-Appropriate Exercises
:Pelvic floor therapy for children involves age-appropriate exercises and techniques to ensure they can understand and perform them correctly.
Therapists use fun and engaging methods to teach children about their pelvic floor muscles and how to control them.
Parental Involvement
:Involving parents in the therapy process is crucial for ensuring consistency and support at home.
Parents can help reinforce exercises, manage fluid intake, and establish healthy bathroom habits.
Conclusion
Pelvic floor therapy offers a comprehensive approach to managing bedwetting by addressing the muscular and behavioral aspects of bladder control. Through strengthening exercises, biofeedback training, bladder training, and behavioral interventions, pelvic floor therapy can significantly reduce the frequency of bedwetting episodes and improve overall bladder function. For children, incorporating fun and engaging exercises, along with parental involvement, can enhance the effectiveness of the therapy and support long-term success in achieving dry nights. Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment