Back
IBS vs. IBD? Exploring Complications and the Role of Pelvic Floor Physical Therapy
By Dr. Christine Martirez PT, DPT on 3/8/2024
Digestive disorders can significantly impact one's quality of life, and among the myriad of conditions, Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) stand out. While both share some symptoms, they are distinct conditions with varying causes and treatment approaches. In this blog post, we'll delve into the differences between IBS and IBD, focusing on two prevalent forms of IBD—Crohn's disease and Ulcerative Colitis. Additionally, we'll explore the common complications associated with IBD and discuss how pelvic floor physical therapy can offer relief.
Understanding IBS vs. IBD
Irritable Bowel Syndrome (IBS):
IBS is a functional gastrointestinal disorder characterized by symptoms like abdominal pain, bloating, and altered bowel habits without any structural damage or inflammation in the digestive tract.
Its exact cause remains unknown, but factors such as stress, diet, and gut-brain axis dysfunction may contribute.
Inflammatory Bowel Disease (IBD):
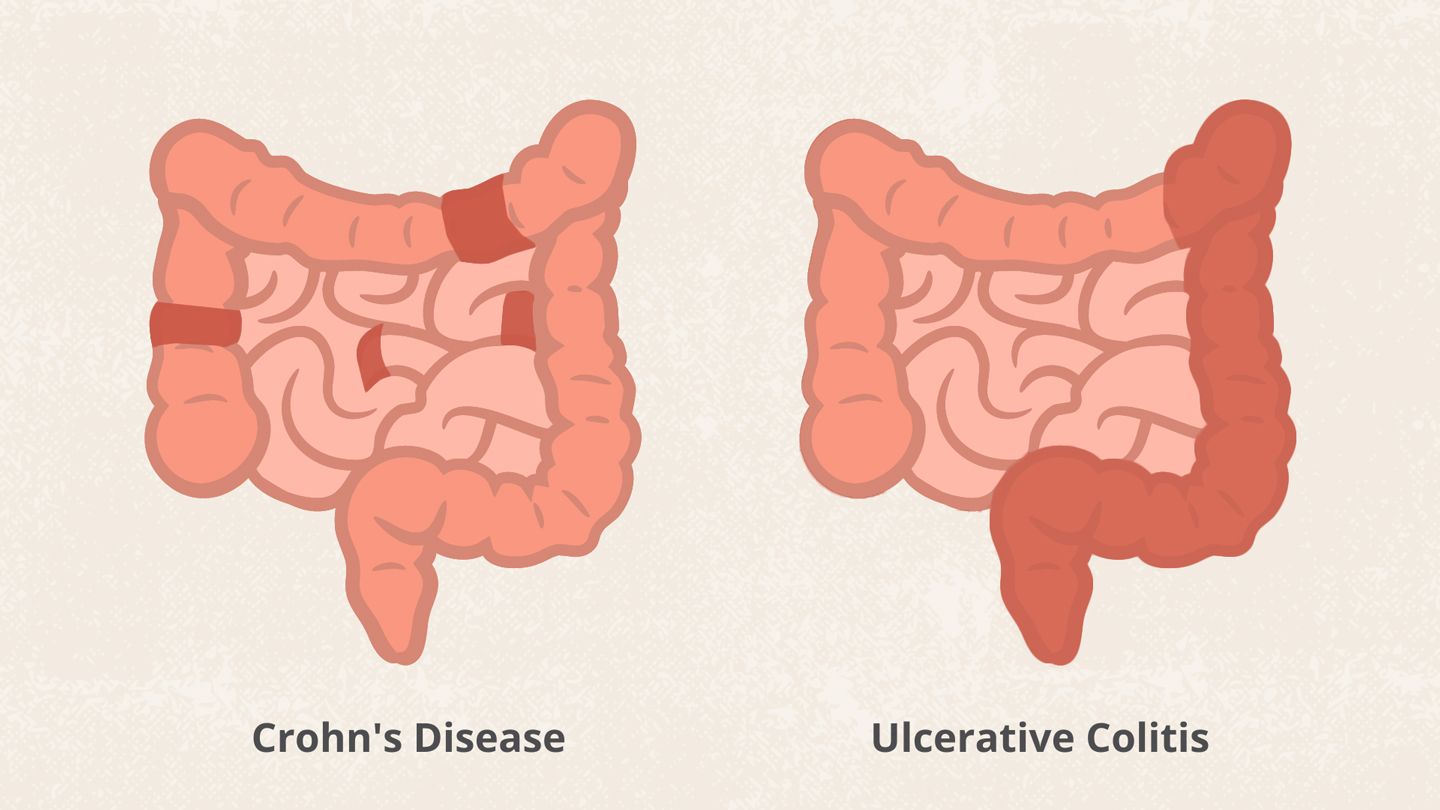
IBD encompasses chronic conditions involving inflammation of the digestive tract, with two primary forms being Crohn's disease and Ulcerative Colitis.
Crohn's disease can affect any part of the digestive tract and is known for its transmural inflammation, while Ulcerative Colitis primarily affects the colon and rectum with continuous mucosal inflammation.
Differentiating Crohn's Disease and Ulcerative Colitis
Crohn's Disease:
Can affect any part of the gastrointestinal tract, from mouth to anus.
May experiences patches inflamed intestine interspersed with areas of healthy intestine.
Inflammation can penetrate through multiple layers of the bowel wall.
Ulcerative Colitis:
Limited to the colon and rectum.
Inflammation typically starts in the rectum and progresses continuously along the colon.
May lead to ulcers on the colon's inner lining.

Common Complications of IBD
Fecal Incontinence and Urgency:
Inflammation and damage to the rectum can lead to loss of bowel control.
Nighttime Soiling:
Frequent urgency and incontinence during sleep can disrupt sleep patterns.
Urinary Incontinence:
Inflammation and pressure on the pelvic floor can affect bladder function.
Abdominal Pain:
Persistent pain due to inflammation and complications like strictures.
Hip and Core Weakness:
Reduced physical activity and nutrient malabsorption can contribute to muscle weakness.
Pelvic Pain:
Inflammation in the pelvic area can cause chronic pain.
Fatigue:
Chronic inflammation and nutrient deficiencies can lead to fatigue.
Osteoporosis and Sarcopenia:
Malabsorption of nutrients may contribute to bone and muscle loss.

Role of Pelvic Floor Physical Therapy
Pelvic floor physical therapy is an emerging and effective approach to address complications associated with IBD. Our therapists work to strengthen and relax the muscles of the pelvic floor, aiding in better bowel and bladder control. Techniques such as biofeedback, therapeutic exercises, manual therapy, myofascial release, visceral mobilization, and relaxation techniques can alleviate symptoms and improve overall quality of life for individuals with IBD.

Navigating the complexities of IBS and IBD, particularly Crohn's disease and Ulcerative Colitis, requires a comprehensive understanding of their differences and associated complications. Pelvic floor physical therapy emerges as a promising non-invasive approach to managing various symptoms, enhancing the well-being of individuals living with these challenging conditions. If you’re experiencing complications from IBS or IBD, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment