Back
Managing Rectal Pain with Pelvic Floor Physical Therapy
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 10/29/2023
Overview
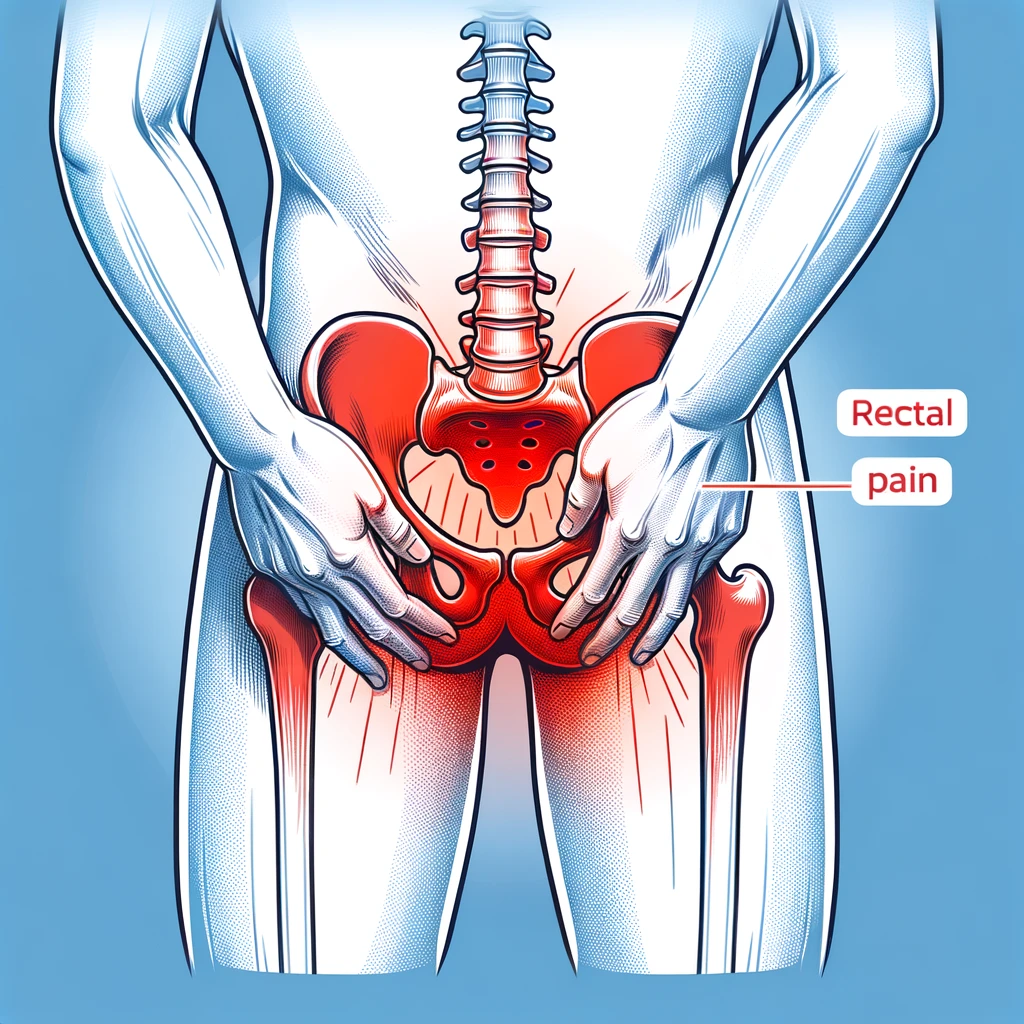
Rectal pain is a common issue that can greatly impact a person's quality of life. It can be caused by a variety of factors such as constipation, hemorrhoids, or pelvic floor dysfunction. In this article, we will focus on the role of pelvic floor dysfunction in rectal pain and how pelvic floor physical therapy can help alleviate symptoms.
Explanation of Rectal Pain
Rectal pain is a discomfort or pain felt in the rectum, which is the final portion of the large intestine that connects to the anus. It can range from mild discomfort to severe pain and can be accompanied by other symptoms such as itching, burning, or bleeding. The causes of rectal pain can vary, but it is often associated with issues in the pelvic floor muscles.
Importance of Addressing Pelvic Floor Dysfunction
The pelvic floor muscles play a crucial role in supporting the organs in the pelvis, including the bladder, uterus, and rectum. When these muscles are weak or tight, it can lead to pelvic floor dysfunction, which can cause a variety of symptoms, including rectal pain. It is essential to address pelvic floor dysfunction to not only alleviate symptoms but also prevent further complications.
Introduction to Pelvic Floor Physical Therapy
Pelvic floor physical therapy is a specialized form of therapy that focuses on the muscles, ligaments, and connective tissues in the pelvic region. It involves exercises, stretches, and other techniques to help improve the strength, flexibility, and coordination of the pelvic floor muscles. This can help alleviate symptoms of rectal pain and improve overall pelvic floor function.
Causes of Rectal Pain
Anal Fissures
Anal fissures are small tears in the lining of the anus that can cause intense pain during bowel movements. They are often caused by constipation, diarrhea, or trauma to the anal area. The pain from anal fissures can be sharp and burning, and may also be accompanied by bleeding.
Hemorrhoids
Hemorrhoids are swollen veins in the rectum and anus that can cause discomfort and pain. They can be internal or external, and are often caused by straining during bowel movements, pregnancy, or chronic constipation. Hemorrhoids can also cause bleeding and itching in the anal area.
Proctitis
Proctitis is inflammation of the lining of the rectum, which can cause rectal pain and discomfort. It can be caused by infections, inflammatory bowel disease, or radiation therapy. Symptoms may include rectal bleeding, diarrhea, and pain during bowel movements.
Pelvic Floor Muscle Dysfunction
Pelvic floor muscle dysfunction occurs when the muscles in the pelvic floor are too tight or too weak, leading to pain and discomfort in the rectal area. This can be caused by chronic constipation, childbirth, or pelvic surgery. Pelvic floor physical therapy can help to relax and strengthen these muscles, relieving rectal pain.
Other Underlying Conditions
Rectal pain can also be caused by other underlying conditions such as anal abscesses, anal cancer, or inflammatory bowel disease. It is important to consult with a healthcare professional to determine the underlying cause of rectal pain and develop an appropriate treatment plan.
Symptoms of Pelvic Floor Dysfunction
Pain in the Rectum or Pelvic Area
Pelvic floor dysfunction can cause pain in the rectum or pelvic area. This pain may be constant or intermittent and can range from mild discomfort to severe pain. It may also be accompanied by a feeling of pressure or fullness in the rectum or pelvic area. This pain can make it difficult to sit or engage in daily activities, and may also be worsened by certain movements or positions.
Difficulty with Bowel Movements
The pelvic floor muscles play a crucial role in bowel movements, and dysfunction in these muscles can lead to difficulty with bowel movements. This can manifest as constipation, straining during bowel movements, or a feeling of incomplete evacuation. In some cases, pelvic floor dysfunction can also cause fecal incontinence, where a person experiences involuntary leakage of stool.
Urinary Incontinence
The pelvic floor muscles also help control bladder function, and dysfunction in these muscles can lead to urinary incontinence. This can manifest as leakage of urine with activities such as coughing, sneezing, or laughing, or a sudden and strong urge to urinate that is difficult to control. Pelvic floor physical therapy can help strengthen these muscles and improve bladder control.
Sexual Dysfunction
Pelvic floor dysfunction can also affect sexual function. In women, it can lead to pain during intercourse, difficulty achieving orgasm, or decreased sexual desire. In men, it can cause erectile dysfunction or pain during ejaculation. These symptoms can greatly impact a person's quality of life and can be addressed through pelvic floor physical therapy.
Other Associated Symptoms
In addition to the above symptoms, pelvic floor dysfunction may also be associated with other symptoms such as pelvic pain, lower back pain, hip pain, and muscle spasms in the pelvic region. It may also contribute to conditions such as interstitial cystitis, endometriosis, and vulvodynia. Identifying and addressing pelvic floor dysfunction can help alleviate these associated symptoms and improve overall pelvic health.
Diagnosis of Pelvic Floor Dysfunction
Physical Examination
A physical examination is an important first step in diagnosing pelvic floor dysfunction. During this exam, a healthcare provider will assess the external and internal structures of the pelvic floor, including the muscles, nerves, and connective tissue. They may also perform a digital rectal exam to check for any abnormalities or tension in the pelvic floor muscles.
Medical History
In addition to a physical exam, a thorough medical history is crucial in diagnosing pelvic floor dysfunction. This may include questions about symptoms, past medical conditions, and any previous pelvic surgeries or trauma. It is important for patients to be open and honest about their symptoms and medical history in order to receive an accurate diagnosis.
Pelvic Floor Muscle Assessment
A pelvic floor muscle assessment is a specific evaluation of the strength, tone, and coordination of the pelvic floor muscles. This may be done through a combination of manual muscle testing and biofeedback techniques. The results of this assessment can help determine if there is any dysfunction or weakness in the pelvic floor muscles.
Diagnostic Tests
In some cases, additional diagnostic tests may be necessary to fully evaluate pelvic floor dysfunction. These may include anorectal manometry, which measures the pressure and function of the rectum and anal sphincter muscles, and defecography, which uses X-rays to assess the function of the rectum and pelvic floor muscles during defecation. These tests can provide valuable information about the underlying causes of rectal pain and help guide treatment.
Pelvic Floor Physical Therapy
Explanation of the Treatment Approach
Pelvic floor physical therapy is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues in the pelvic region. The goal of this treatment approach is to address issues such as rectal pain, incontinence, and pelvic floor dysfunction. The therapist will work with the patient to identify any underlying causes of their symptoms and develop a personalized treatment plan.
Techniques Used
There are several techniques used in pelvic floor physical therapy, including biofeedback, manual therapy, and exercises. Biofeedback involves using sensors to monitor muscle activity and provide visual or auditory feedback to the patient. This can help them learn how to control and relax their pelvic floor muscles. Manual therapy involves hands-on techniques to release tension and improve muscle function. Exercises may include strengthening, stretching, and relaxation techniques.
Importance of Proper Breathing and Relaxation Techniques
Breathing and relaxation techniques are crucial in pelvic floor physical therapy. These techniques can help patients learn how to relax their pelvic floor muscles, which can be beneficial for conditions such as rectal pain. Proper breathing techniques can also help with pain management and improve overall muscle function in the pelvic region.
Duration and Frequency of Therapy Sessions
The duration and frequency of pelvic floor physical therapy sessions will vary depending on the individual's needs and goals. Typically, sessions last for 30-60 minutes and may be scheduled once or twice a week. The length of treatment may also vary, with some patients seeing improvement in a few weeks, while others may require several months of therapy.
Benefits and Success of Pelvic Floor Physical Therapy
Improvement in Symptoms
Pelvic floor physical therapy has been shown to significantly improve symptoms related to rectal pain. This can include pain during bowel movements, discomfort or pressure in the rectal area, and difficulty with bowel control. Through targeted exercises and techniques, pelvic floor physical therapy can help to strengthen and relax the muscles in the pelvic floor, leading to a reduction in symptoms.
Increased Quality of Life
Chronic rectal pain can greatly impact a person's quality of life, causing discomfort and embarrassment. Pelvic floor physical therapy can help to improve overall pelvic floor function, leading to a better quality of life. This can include improved bowel control, reduced pain and discomfort, and increased confidence and comfort in daily activities.
Avoidance of Invasive Procedures
Pelvic floor physical therapy can often be an effective alternative to invasive procedures, such as surgery, for treating rectal pain. By addressing the root cause of the pain and working to improve pelvic floor function, physical therapy can help to avoid the need for more invasive treatments. This can also lead to a faster recovery time and fewer potential complications.
Success Rates and Patient Satisfaction
Studies have shown that pelvic floor physical therapy has a high success rate in treating rectal pain. Many patients report significant improvements in their symptoms and overall satisfaction with the treatment. This can be attributed to the personalized and non-invasive approach of physical therapy, as well as the focus on long-term management and maintenance of pelvic floor health.
Long-Term Management and Maintenance of Pelvic Floor Health
Pelvic floor physical therapy not only addresses current symptoms, but also focuses on long-term management and maintenance of pelvic floor health. This can include exercises and techniques to strengthen and relax the pelvic floor muscles, as well as education on proper bowel habits and posture. By maintaining a healthy pelvic floor, patients can reduce the risk of future rectal pain and related issues.
If you are experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment