Back
Physical Therapy for Pelvic Pain Treatment and Addressing Chronic Pelvic Pain
By Dr. Christine Martirez PT, DPT on 5/30/2024

Pelvic pain is a complex and often debilitating condition that can affect both men and women. It can arise from various sources, including injury, muscle dysfunction, gynecological conditions, bladder disorders, infections, and gastrointestinal issues. This blog post will explore common causes of pelvic pain, the functions of the pelvic floor muscles, and how pelvic floor physical therapy can help evaluate and treat this condition.
Common Causes of Pelvic Pain
Injury to the Area:
Trauma or injury to the pelvic region, such as from a fall, surgery, or childbirth, can lead to persistent pain and dysfunction.
Pelvic Floor Muscle Dysfunction:
Overactive or underactive pelvic floor muscles can cause pain, discomfort, and issues with bladder and bowel control.
Endometriosis:
A condition where tissue similar to the lining of the uterus grows outside the uterus, causing severe pain, especially during menstruation.
Bladder Disorders:
Conditions such as interstitial cystitis or painful bladder syndrome can cause chronic pelvic pain and urinary discomfort.
Sexually Transmitted Infections (STIs):
Infections like chlamydia, gonorrhea, and herpes can lead to inflammation and pain in the pelvic area.
Constipation:
Chronic constipation can strain the pelvic floor muscles and cause pain due to pressure and discomfort in the pelvic region.
Other Conditions:
Fibroids, ovarian cysts, pelvic inflammatory disease (PID), and irritable bowel syndrome (IBS) are other conditions that can contribute to pelvic pain.
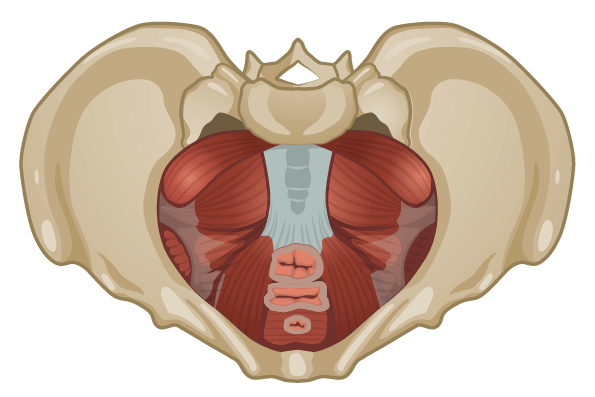
The Pelvic Floor Muscles and Their Functions
The pelvic floor muscles are a group of muscles that span the bottom of the pelvis, forming a supportive hammock for the pelvic organs. These muscles are crucial for several bodily functions, often summarized by the "5 S's":
Sexual Function:
The pelvic floor muscles play a key role in sexual arousal and orgasm. They contract rhythmically during orgasm, contributing to sexual pleasure.
Stability:
These muscles help stabilize the pelvis and spine, working in coordination with the core muscles to maintain posture and support movements.
Sump Pump:
The pelvic floor muscles assist in venous and lymphatic return from the lower body, helping to prevent swelling and improve circulation.
Support:
They provide support for the pelvic organs, including the bladder, uterus, and rectum, preventing conditions like prolapse.
Sphincteric Function:
The muscles control the openings of the bladder and bowel, playing a critical role in continence by contracting to retain urine and feces and relaxing to allow for their passage.
How Pelvic Floor Physical Therapy Can Help
Pelvic floor physical therapy (PFPT) is a specialized form of physical therapy aimed at treating dysfunction in the pelvic floor muscles. Here’s how PFPT can help evaluate and treat conditions causing pelvic pain:
Comprehensive Evaluation:
A pelvic floor physical therapist conducts a thorough evaluation, including a medical history review, physical examination, postural assessment, and assessment of pelvic floor muscle function and surrounding musculature. This helps identify the underlying cause of pelvic pain.
Manual Therapy:
Hands-on techniques such as myofascial release, trigger point therapy, and soft tissue mobilization can help alleviate pain, reduce muscle tension, and improve mobility in the pelvic region.
Pelvic Floor Exercises:
Customized exercise programs are designed to strengthen or relax the pelvic floor muscles, depending on the specific dysfunction. Exercises may include pelvic floor contractions (Kegels) for strengthening, reverse Kegels for relaxation, postural re-education, and strength and mobility through surrounding musculature.
Biofeedback:
Biofeedback can help provide tactile feedback on pelvic floor muscle activity, helping patients learn how to properly contract and relax these muscles.
Behavioral Modification:
Therapists provide education on lifestyle and behavioral changes to reduce pain and prevent exacerbation of symptoms. This may include advice on proper body mechanics, bladder and bowel habits, and stress management techniques.
Pain Management Techniques:
PFPT may include the use of modalities such as heat, cold, electrical stimulation, and relaxation techniques to manage pain and reduce inflammation.
Coordination with Other Healthcare Providers:
Pelvic floor physical therapists often work in collaboration with other healthcare providers, including gynecologists, urologists, gastroenterologists, and pain specialists, to provide comprehensive care for conditions like endometriosis, bladder disorders, and constipation.
Pelvic pain can stem from various causes, including injury, muscle dysfunction, gynecological and bladder conditions, infections, and gastrointestinal issues. Understanding the role of the pelvic floor muscles and their functions is essential in addressing these issues. Pelvic floor physical therapy offers a holistic and effective approach to evaluating and treating pelvic pain, employing techniques such as manual therapy, pelvic floor exercises, biofeedback, and behavioral modifications. By addressing the root causes and providing targeted interventions, pelvic floor physical therapy can significantly improve the quality of life for individuals suffering from pelvic pain.
Are you suffering from pelvic pain? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment