Back
The TMJ-Pelvic Floor Connection
By Shannon Strauch, PTA, STMT-1 on 11/5/2024
The jaw (temporomandibular joint or TMJ) and the pelvic floor may seem distant in the body, but they are surprisingly connected. This connection is rooted in our body’s intricate anatomy, involving fascial lines, embryologic development, the effects of chronic stress, and the vagus nerve. Understanding this relationship can provide insights into how dysfunction in one area, like the TMJ, might affect the pelvic floor and vice versa.
1. Fascial Lines: The Anatomy Connection
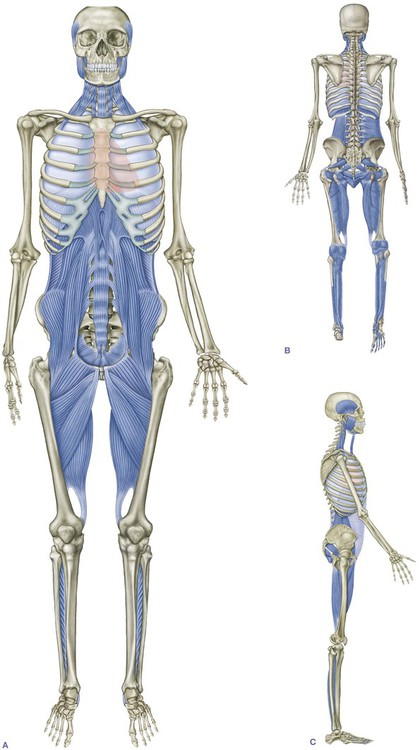
The body is connected by fascial lines—web-like structures of connective tissue that encase muscles, bones, and organs, creating continuous pathways from head to toe. Fascial lines distribute tension and pressure throughout the body, helping muscles and organs work in sync. The “Deep Front Line” (DFL), as described by anatomist Tom Myers, is one of the most notable fascial lines that connects the pelvic floor with areas further up the body, including the jaw.
The DFL starts at the feet, travels up through the inner thighs, pelvis, and spine, and connects to the muscles around the ribcage and up to the jaw. Tension along this line can impact multiple areas, including the pelvic floor and the TMJ. When one part of the DFL becomes tight or dysfunctional, it can cause compensatory tension or strain in other parts. For example, clenching the jaw might contribute to tension in the pelvis, affecting the stability and function of the pelvic floor.
2. Embryologic Development: Connections from Conception
Embryologic development sheds light on the TMJ-pelvic floor connection. During early development, structures that will eventually form the jaw, neck, diaphragm, and pelvic floor originate from nearby regions of the embryonic tissue. This shared origin could explain why these regions retain a "communication line" even as the body grows and differentiates.
This development pattern may also mean that certain reflexes and tension patterns are retained between these areas. For instance, the body can hold onto tension as a protective response to stress or trauma, and this can manifest in both the jaw and pelvic regions. Addressing these connections holistically can help release these embedded patterns.

3. Chronic Stress and Tension: The Body’s Protective Response
Chronic stress affects both the TMJ and pelvic floor, often by leading to tension and dysfunctional holding patterns. When we experience stress, our body responds by clenching muscles in areas associated with fight-or-flight responses. Jaw clenching and pelvic floor gripping are common responses to ongoing stress, and over time, this can contribute to TMJ disorder or pelvic floor dysfunction.
Stress also promotes shallow breathing, which fails to fully engage the diaphragm and pelvic floor muscles, weakening their functionality over time. Chronic clenching can lead to myofascial pain in both the jaw and pelvic floor, reinforcing dysfunction and discomfort.
4. The Role of the Vagus Nerve: A Vital Regulator
The vagus nerve, the longest cranial nerve in the body, plays a key role in the relaxation response. This nerve connects the brainstem to many body organs, including the heart, lungs, and digestive system, and it influences muscle tone in the neck, jaw, and pelvic floor. When the vagus nerve is activated, it promotes a relaxation response, which helps decrease muscle tension in these areas.
For people with chronic TMJ or pelvic floor dysfunction, vagal stimulation techniques (like diaphragmatic breathing, humming, or certain relaxation exercises) may help reduce muscle tension and pain by activating the parasympathetic nervous system. This can lead to improvements in both jaw and pelvic floor symptoms, emphasizing how essential this nerve is for achieving muscle relaxation and reducing pain.
Integrating TMJ and Pelvic Floor Therapy
Given the connections between the TMJ and pelvic floor, addressing one area may benefit the other. Therapies like fascial counterstrain, myofascial release, or targeted exercises focusing on vagal nerve activation can help relieve tension across these regions. For people struggling with either TMJ or pelvic floor issues, recognizing this interconnectedness may open up new therapeutic options.
Understanding the jaw-pelvic floor connection, rooted in our body’s structural, developmental, and neurological makeup, offers a pathway to more holistic approaches in treating these dysfunctions. Looking to optimize your well being with pelvic floor physical therapy? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment