Back
Understanding Diastasis Recti (DRA)
By Shannon Strauch, PTA, STMT-1 on 10/31/2024
Understanding Diastasis Recti: Its Impact on Bloating, Low Back Pain, Urinary Incontinence, and How Pelvic Floor Therapy Can Help
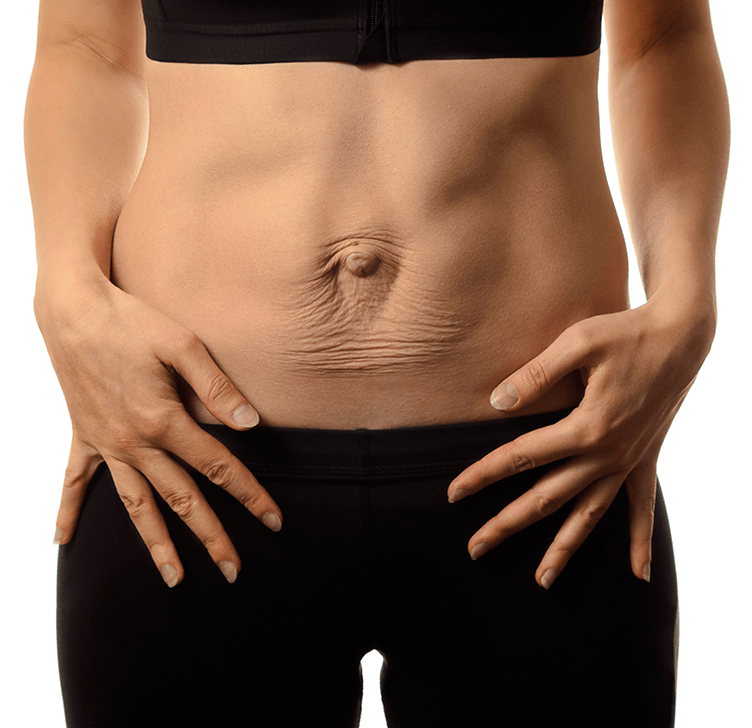
Diastasis recti abdominis (DRA), commonly known as abdominal separation, is a condition in which the connective tissue (linea alba) that connects the left and right sides of the rectus abdominis muscles stretches or thins, often due to the pressure of pregnancy. This separation can weaken core stability, impact posture, and affect several other systems, contributing to symptoms like bloating, low back pain, and urinary incontinence. Here, we’ll dive into how DRA impacts these issues and explore how pelvic floor therapy can support recovery.
1.
Bloating and Digestive Discomfort
With diastasis recti, the weakened abdominal muscles can struggle to support the digestive organs, impacting digestion and sometimes leading to bloating or discomfort. This may be especially noticeable after meals or physical activity. Poorly supported abdominal organs can also affect peristalsis, the process by which food moves through the intestines, leading to constipation or irregular digestion.
How Pelvic Floor Therapy Can Help:
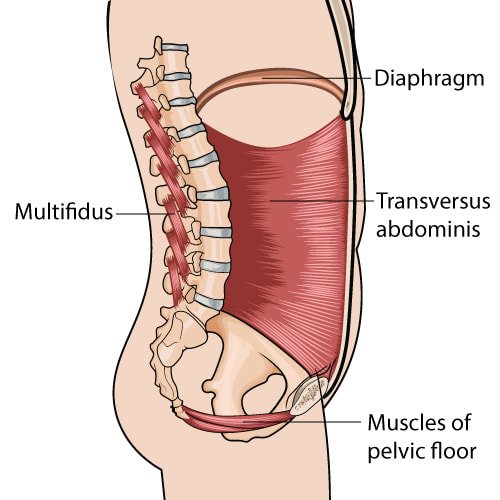
Pelvic floor therapy strengthens the deeper core muscles, particularly the transverse abdominis, which is essential for stabilizing the torso and supporting digestion. Targeted exercises can also help restore the alignment and functionality of the entire core, promoting better digestive health and reducing bloating.2.
Low Back Pain and Posture Issues
When the rectus abdominis muscles are weakened by DRA, the back muscles often take on more strain to compensate. This can contribute to low back pain, especially with prolonged standing, lifting, or even everyday movements. Over time, poor alignment and muscular compensation patterns can worsen, creating a cycle of back discomfort and muscle fatigue.
How Pelvic Floor Therapy Can Help:
Pelvic floor therapy works to engage and strengthen the core as a whole, particularly the pelvic floor and deep abdominal muscles, which are critical for balanced posture. Therapy can retrain the body to use these stabilizing muscles, taking pressure off the back and realigning the body for optimal posture. This improved posture can lessen strain on the back, reducing pain and improving functional strength.3.
Urinary Incontinence
Diastasis recti is linked to reduced pelvic floor support, which is essential for bladder control. The interconnectedness of core muscles means that weakness in one area, like the abdominal wall, can have a direct effect on the pelvic floor. For many people, this manifests as urinary incontinence, especially during activities that increase abdominal pressure, like sneezing, laughing, or exercising.
How Pelvic Floor Therapy Can Help:
Pelvic floor therapy addresses the deep core connection, using targeted exercises to strengthen not only the pelvic floor but also the entire abdominal support system. Therapists often teach diaphragmatic breathing, core coordination exercises, and specific pelvic floor contractions to improve bladder control, providing relief from stress incontinence associated with DRA.Additional Benefits of Pelvic Floor Therapy for DRA Recovery
Beyond the specific symptoms of bloating, back pain, and incontinence, pelvic floor therapy helps address DRA holistically. Therapists can tailor exercises to an individual’s needs, gradually progressing to include functional movements and strength-building, leading to better movement and stability in everyday activities.
Final Thoughts
If you’re experiencing the symptoms of diastasis recti, addressing them through pelvic floor therapy can be a game-changer. Working with a pelvic floor therapist can help you rebuild the deep core muscles and regain strength, stability, and control. Over time, this holistic approach to managing DRA not only alleviates symptoms but also supports a strong, functional core for the long term.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment