Back
Understanding Male Urinary Incontinence
By Shannon Strauch, PTA, STMT-1 on 7/30/2024

Urinary incontinence in men is a prevalent yet often under-discussed issue. It can significantly impact quality of life, but understanding its causes and available treatments can provide a pathway to managing this condition effectively. This blog explores why male urinary incontinence occurs, the role of pelvic musculature and coordination, and how pelvic floor therapy can be a beneficial treatment option.
Causes of Male Urinary Incontinence
Prostate Issues
:Enlarged Prostate (BPH)
: Benign Prostatic Hyperplasia can obstruct urine flow, leading to leakage.
Prostate Surgery
: Procedures like prostatectomy can damage the muscles and nerves involved in urinary control.
Neurological Conditions
:Parkinson's Disease
: Affects the brain's ability to control bladder function.
Multiple Sclerosis
: Can disrupt nerve signals between the bladder and brain.
Spinal Cord Injury
: Can sever the communication between the brain and bladder, leading to incontinence.
Pelvic Muscle Weakness
:Poor Coordination
: Inability of pelvic floor muscles to contract or relax properly.
Reduced Strength
: Weakened muscles can't support the bladder adequately.
Medications
:Some drugs, especially diuretics and certain antidepressants, can affect bladder control.
Lifestyle Factors
:Obesity
: Excess weight can put pressure on the bladder.
Smoking
: Can lead to chronic coughing, which strains the pelvic floor.
Chronic Constipation
: Straining during bowel movements weakens pelvic floor muscles.
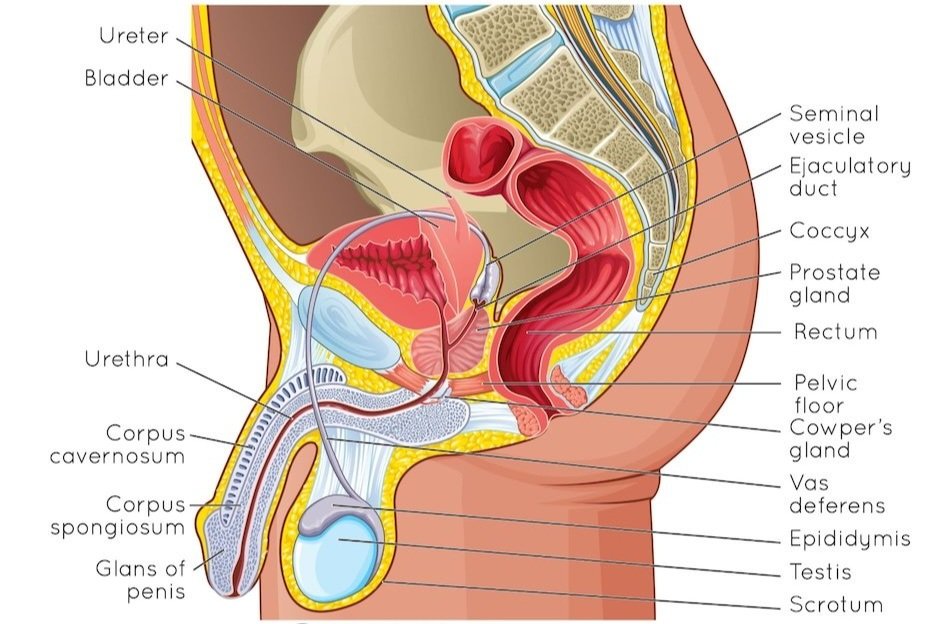
Musculature and Coordination Involved
Pelvic Floor Muscles
: These muscles support the bladder and bowel and play a critical role in maintaining continence.
Sphincter Function
: The external urinary sphincter controls the release of urine from the bladder. Damage or weakening of this muscle can lead to leakage.
Neuromuscular Coordination
: Effective bladder control depends on the precise communication between nerves and muscles. Any disruption in this communication can result in incontinence.
How Pelvic Floor Therapy Can Help
Pelvic floor therapy offers a comprehensive approach to managing urinary incontinence by addressing the underlying muscular and coordination issues.
Assessment and Diagnosis
:A pelvic floor therapist conducts a thorough evaluation to identify specific weaknesses and coordination problems.
Targeted Exercises
:Kegels
: Strengthening exercises focused on contracting and relaxing the pelvic floor muscles.
Functional Training
: Exercises that incorporate pelvic floor muscle use in daily activities.
Behavioral Techniques
:Bladder Training
: Techniques to extend the time between urinations and increase bladder capacity.
Urgency Control Strategies
: Methods to reduce the feeling of urgency and prevent accidents.
Education and Lifestyle Changes
:Diet and Fluid Intake
: Guidance on avoiding bladder irritants and maintaining a healthy fluid intake.
Healthy Habits
: Tips on weight management, quitting smoking, and managing constipation.
Conclusion
Male urinary incontinence is a multifaceted issue with several underlying causes, often related to the pelvic floor's strength and coordination. Pelvic floor therapy provides targeted interventions that address these issues, offering hope and improved quality of life for those affected. By understanding the condition and seeking appropriate treatment, many men can regain control and confidence. Looking to optimize your well being with pelvic floor physical therapy? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment