Back
Understanding Prostatitis
By Shannon Strauch, PTA, STMT-1 on 10/1/2024
Prostatitis is a common yet often misunderstood condition that affects men of all ages. While it’s typically associated with bacterial infections, not all cases are caused by bacteria. In fact, many men experience symptoms that don’t resolve with antibiotics, leading to confusion and frustration. Let’s dive into what prostatitis is, why antibiotics might not always work, and how pelvic floor therapy can play a crucial role in treatment.
What is Prostatitis?
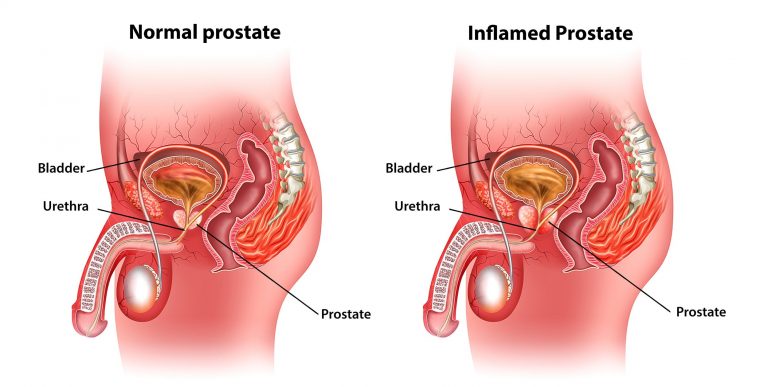
Prostatitis is the inflammation of the prostate gland, which can lead to various urinary, pelvic, and sexual symptoms. There are several types of prostatitis, each with different causes and treatment strategies:
Acute Bacterial Prostatitis
: A sudden bacterial infection that causes severe symptoms like fever, chills, painful urination, and pelvic pain. This type often responds well to antibiotics.Chronic Bacterial Prostatitis
: A longer-term bacterial infection that may cause recurring urinary tract infections (UTIs). Symptoms come and go and may improve temporarily with antibiotics.Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
: This is the most common form of prostatitis. Unlike bacterial prostatitis, there is often no clear infection, yet the symptoms—pelvic pain, urinary problems, and sexual dysfunction—are persistent. Antibiotics usually have little or no effect.Asymptomatic Inflammatory Prostatitis
: In this type, men have no symptoms, but inflammation is detected during other medical evaluations, often discovered during a prostate biopsy.
Symptoms of Prostatitis
Prostatitis can manifest through a wide range of symptoms, which often vary in severity depending on the type. Common symptoms include:
Pain or discomfort in the pelvic area, groin, or lower back
Frequent, urgent need to urinate
Painful or difficult urination
Pain during or after ejaculation
Erectile dysfunction or reduced sexual function
Fatigue and feelings of depression due to chronic discomfort
In cases where antibiotics don’t resolve the symptoms, it’s crucial to look beyond infection and explore other potential causes.
Why Antibiotics Might Not Always Work
While antibiotics are the go-to treatment for bacterial prostatitis, they are ineffective for non-bacterial cases such as
chronic pelvic pain syndrome (CPPS)
. In these instances, there is no bacterial infection to treat. The problem often lies within thepelvic floor muscles
, which can become tense, irritated, or dysfunctional due to stress, poor posture, or previous infections.If antibiotics don’t work and you’re still experiencing pelvic discomfort, it may be time to consider that tight or overactive pelvic floor muscles could be at the root of your pain.
How Pelvic Floor Dysfunction Contributes to Prostatitis
The pelvic floor is a group of muscles that support the bladder, bowel, and prostate, playing a key role in urinary control and sexual function. When these muscles are overly tight or strained, they can cause significant pelvic pain and dysfunction, mimicking the symptoms of prostatitis.
Pelvic floor dysfunction
can result from several factors:Prolonged sitting or poor posture
Stress and anxiety, leading to muscle tension
Physical strain from heavy lifting or intense exercise
Previous injuries or infections
Scar tissue from surgeries or trauma
When these muscles are tense, they can compress the prostate and surrounding nerves, causing the pelvic pain, urinary issues, and sexual problems often attributed to prostatitis.
How Pelvic Floor Therapy Can Help
If your prostatitis symptoms persist despite antibiotics, pelvic floor therapy may be the key to relief. Pelvic floor physical therapy involves specialized techniques aimed at restoring normal function to the pelvic muscles and relieving tension. Here’s how it works:
1.
Muscle Assessment
A pelvic floor therapist will assess the strength, flexibility, and coordination of your pelvic floor muscles. Tight or weak muscles can often be identified as the source of pain.
2.
Manual Therapy
Hands-on techniques like trigger point release, myofascial release, and soft tissue mobilization are used to reduce muscle tension and ease pain in the pelvic area. This can help release the muscle knots that contribute to chronic pain.
3.
Relaxation Exercises
Pelvic floor therapy includes exercises to improve relaxation of the pelvic muscles. This may involve diaphragmatic breathing, stretches, and techniques to help you control and relax the muscles of the pelvic floor.
4.
Biofeedback
Biofeedback is used to help you become more aware of your pelvic floor muscles and learn how to control them effectively. It can be particularly useful in teaching muscle relaxation, especially if tightness is contributing to your symptoms.
5.
Posture and Movement Correction
Therapists also work on improving posture and body mechanics. Poor posture, especially sitting for long periods, can contribute to pelvic floor tension, so addressing these habits can reduce strain on the pelvic muscles.
Real Results from Pelvic Floor Therapy
Many men who have been diagnosed with prostatitis, particularly CP/CPPS, have found significant relief through pelvic floor therapy. Even if antibiotics have failed to resolve the issue, addressing muscle tension through physical therapy can lead to improved quality of life, reduced pain, and enhanced urinary and sexual function.
Conclusion
Prostatitis can be a complex and frustrating condition, especially when antibiotics don’t provide relief. If your symptoms persist despite conventional treatments, it may be time to consider pelvic floor dysfunction as a contributing factor. Pelvic floor therapy offers a non-invasive and effective approach to managing chronic prostatitis symptoms, addressing the root cause rather than just treating the symptoms.
By seeking out a trained pelvic floor therapist, you can develop a personalized treatment plan that targets muscle tension, promotes relaxation, and restores function to your pelvic floor, bringing much-needed relief and comfort.
If you’re experiencing symptoms of prostatitis that haven’t improved with antibiotics, consider discussing pelvic floor therapy with your healthcare provider. With the right approach, relief may be closer than you think. Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment