Back
Urinary Urgency and Frequency
By Shannon Strauch, PTA, STMT-1 on 6/26/2024
What is Urinary Urgency and Frequency?
Urinary Urgency:
Urinary urgency is a sudden, compelling need to urinate that is difficult to defer. It is often accompanied by a feeling that the bladder must be emptied immediately.
Symptoms of Urinary Urgency:
Sudden and strong urge to urinate
Difficulty delaying urination
Often leads to frequent trips to the bathroom
Causes of Urinary Urgency:
Overactive bladder (OAB)
Urinary tract infections (UTIs)
Bladder irritants (e.g., caffeine, alcohol)
Bladder or pelvic floor dysfunction
Neurological disorders
Bladder inflammation or interstitial cystitis
Urinary Frequency:
Urinary frequency is the need to urinate more often than usual. While the exact number of trips to the bathroom that constitutes urinary frequency can vary, it generally means having to urinate more than 8 times in 24 hours.
Symptoms of Urinary Frequency:
Frequent urination during the day and night (nocturia)
Smaller amounts of urine produced each time
Interruptions to daily activities and sleep due to frequent trips to the bathroom
Causes of Urinary Frequency:
Overactive bladder (OAB)
Urinary tract infections (UTIs)
Increased fluid intake
Diuretic medications
Bladder or pelvic floor dysfunction
Diabetes
Prostate issues in men
Pregnancy
Connection Between Urinary Urgency and Frequency
Both conditions often coexist, especially in cases of overactive bladder or urinary tract infections. The sudden urge to urinate (urgency) usually leads to increased frequency of urination.
Anatomical Reasons for Urinary Urgency and Frequency
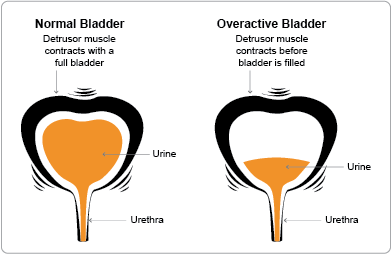
Bladder Overactivity (Overactive Bladder - OAB):
The detrusor muscle (the bladder muscle) contracts involuntarily, leading to a sudden and strong urge to urinate.
This can be due to neurological conditions, aging, or idiopathic causes (unknown reasons).
Bladder Outlet Obstruction:
Blockages at the bladder neck or urethra (e.g., due to prostate enlargement in men, urethral strictures, or pelvic organ prolapse in women) can cause difficulty in emptying the bladder completely, leading to frequent urges.
Interstitial Cystitis (Bladder Pain Syndrome):
Chronic inflammation of the bladder wall can cause pain and a persistent need to urinate.
Urinary Tract Infections (UTIs):
Infections in the urinary tract can irritate the bladder and urethra, leading to urgency and frequency.
Pelvic Floor Dysfunction:
Weakness, tightness, or improper coordination of the pelvic floor muscles can affect bladder function, leading to symptoms of urgency and frequency.
The obturator internus muscle, which forms part of the pelvic floor, can contribute to urinary symptoms if it is tight or weak.
The fascia, a connective tissue network within the pelvic region, can also play a role. Fascia restrictions or adhesions can affect bladder function and lead to urgency and frequency.
Postural Issues:
Poor posture, especially in the thoracic spine (mid-back), can lead to increased pressure on the bladder and pelvic floor. Slouching or excessive forward bending can alter pelvic alignment, leading to urinary urgency and frequency.
How Pelvic Floor Therapy Can Help
Strengthening Pelvic Floor Muscles:
Exercises like Kegels help strengthen the pelvic floor muscles, providing better support for the bladder and improving control over urination.
Relaxation Techniques:
For those with tight or overactive pelvic floor muscles, relaxation techniques, biofeedback, and manual therapy can help reduce muscle tension and improve bladder function.
Techniques specifically targeting the obturator internus can relieve muscle tension and improve bladder function.
Bladder Training:
A physical therapist can guide patients through bladder training programs to gradually increase the time between voiding, reducing the frequency of urination.
Behavioral Modifications:
Education on fluid management, dietary changes, and lifestyle adjustments can help manage symptoms.
Fascial Release:
Manual therapy techniques to release restrictions in the fascia can improve pelvic floor function and reduce urinary symptoms.
Support for Connective Tissue:
Specific exercises and techniques can strengthen and support the structures around the bladder, enhancing bladder control and reducing symptoms of urgency and frequency.
Posture Correction:
Addressing postural issues, particularly in the thoracic spine, can alleviate pressure on the bladder and pelvic floor. Physical therapy can include exercises and stretches to improve posture, reducing the strain on the pelvic region and improving urinary symptoms.
Pelvic floor therapy addresses the underlying muscle issues, connective tissue restrictions, and postural problems, teaching strategies to manage and reduce the symptoms of urinary urgency and frequency, improving the quality of life for those affected. If you or someone you know is struggling with overactive bladder or is always afraid to travel far from a bathroom, reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment