Back
What Is Bladder Retraining?
By Dr. Christine Martirez PT, DPT on 5/28/2024
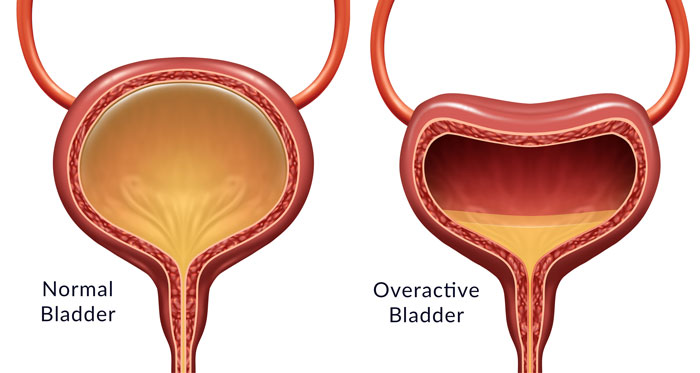
Overactive bladder (OAB) is a common condition characterized by a frequent and urgent need to urinate, sometimes accompanied by incontinence. This condition can significantly impact quality of life, but effective management strategies such as bladder retraining can help. In this blog post, we'll explore the concept of bladder retraining, the role of Bradley's loops in micturition, the involvement of pelvic floor muscles, and how pelvic floor physical therapy can support this process.
Understanding Bradley Loops and Micturition
The process of urination, or micturition, is controlled by a complex interaction of neurological pathways known as Bradley's loops. These loops are essential for the coordination of bladder filling and emptying:
Loop 1 (Pontine Micturition Center to Sacral Micturition Center):
This loop involves signals from the brain's pontine micturition center (PMC) to the sacral micturition center (SMC) in the spinal cord. When the bladder is full, the PMC sends a signal to the SMC to initiate the process of urination.
Loop 2 (Sacral Micturition Center to Bladder and Urethra):
The SMC sends signals to the bladder and urethra. It stimulates the detrusor muscle (bladder muscle) to contract and the internal sphincter to relax, allowing urine to pass.
Loop 3 (Bladder Stretch Receptors to Sacral Micturition Center):
This feedback loop involves stretch receptors in the bladder wall sending signals to the SMC when the bladder is filling. The SMC then communicates with the brain to convey the need to urinate.
Loop 4 (Brain to Pelvic Floor Muscles):
This loop involves voluntary control from the brain to the pelvic floor muscles. The brain can signal the pelvic floor muscles to contract, helping to delay urination until it is convenient.
Disruptions in these loops, such as those caused by neurological conditions, anxiety, or habitual patterns, can contribute to the symptoms of overactive bladder.
How Bladder Retraining Works
Bladder retraining is a behavioral therapy aimed at improving bladder control and reducing the frequency and urgency of urination. It involves gradually increasing the time between voiding and managing the urge to urinate. Here’s how it works:
Scheduled Voiding:
Initially, individuals are advised to follow a voiding schedule, urinating at set intervals (e.g., every hour). Over time, the intervals are gradually extended (e.g., every 1.5 hours, then every 2 hours), helping to train the bladder to hold more urine and reduce the sensation of urgency.
Delayed Urge Response:
When the urge to urinate occurs, individuals practice delaying urination by engaging in distraction techniques or pelvic floor contractions. This helps to increase bladder capacity and decrease sensitivity to urgency.
Fluid and Diet Management:
Adjusting fluid intake and avoiding bladder irritants such as caffeine, alcohol, and spicy foods can help manage symptoms and support bladder retraining efforts.
The Role of Pelvic Floor Muscles
The pelvic floor muscles play a crucial role in bladder control. These muscles support the bladder and urethra, and their proper function is essential for maintaining continence. Here’s how they are involved in bladder retraining:
Pelvic Floor Strength:
Strong pelvic floor muscles help support the bladder and urethra, reducing the likelihood of incontinence. Exercises targeted to pelvic floor muscles and surrounding musculature can help strengthen these muscles.
Voluntary Control:
Contracting the pelvic floor muscles can help suppress the urge to urinate, allowing individuals to delay voiding and adhere to their bladder retraining schedule.
Pelvic Floor Mobility:
Too much tension in the muscles of the pelvic floor can also contribute to higher urinary urgency and frequency. Allowing the muscles to regain an optimal lengthened state can assist in decreasing these symptoms.
Coordination:
Proper coordination between the pelvic floor muscles and the detrusor muscle is essential for effective bladder control. Pelvic floor physical therapy can help improve this coordination.
How Pelvic Floor Physical Therapy Can Help
Pelvic floor physical therapy offers a comprehensive approach to managing overactive bladder and supporting bladder retraining efforts. Here’s how it can help:
Muscle Assessment and Training:
A pelvic floor physical therapist will assess the strength and function of the pelvic floor muscles. They will design a tailored exercise program to strengthen these muscles and improve their coordination.
Biofeedback:
Biofeedback techniques help individuals become aware of their pelvic floor muscle activity and learn how to control them more effectively. This can be particularly helpful in managing urgency and improving bladder control.
Behavioral Strategies:
Therapists provide guidance on bladder retraining techniques, including scheduled voiding and delayed urge response. They also offer strategies for managing fluid intake and avoiding bladder irritants.
Manual Therapy:
Manual therapy techniques can help release tension and improve flexibility in the pelvic floor muscles, supporting overall pelvic health and function.
Education and Support:
Education about bladder function, lifestyle modifications, and coping strategies empowers individuals to take control of their symptoms and improve their quality of life.
Bladder retraining is an effective approach to managing overactive bladder by gradually increasing the time between voiding and improving bladder control. Understanding the role of Bradley loops in micturition and the involvement of pelvic floor muscles is essential for successful bladder retraining. Pelvic floor physical therapy provides a holistic and supportive approach to this process, offering muscle assessment, training, biofeedback, behavioral strategies, manual therapy, and education. By working with a skilled pelvic floor physical therapist, individuals with overactive bladder can achieve better control, reduced symptoms, and an improved quality of life.
Suffering from urinary urgency and frequency? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment