Back
Why am I Having Pain with Sitting?
By Shannon Strauch, PTA, STMT-1 on 10/12/2023
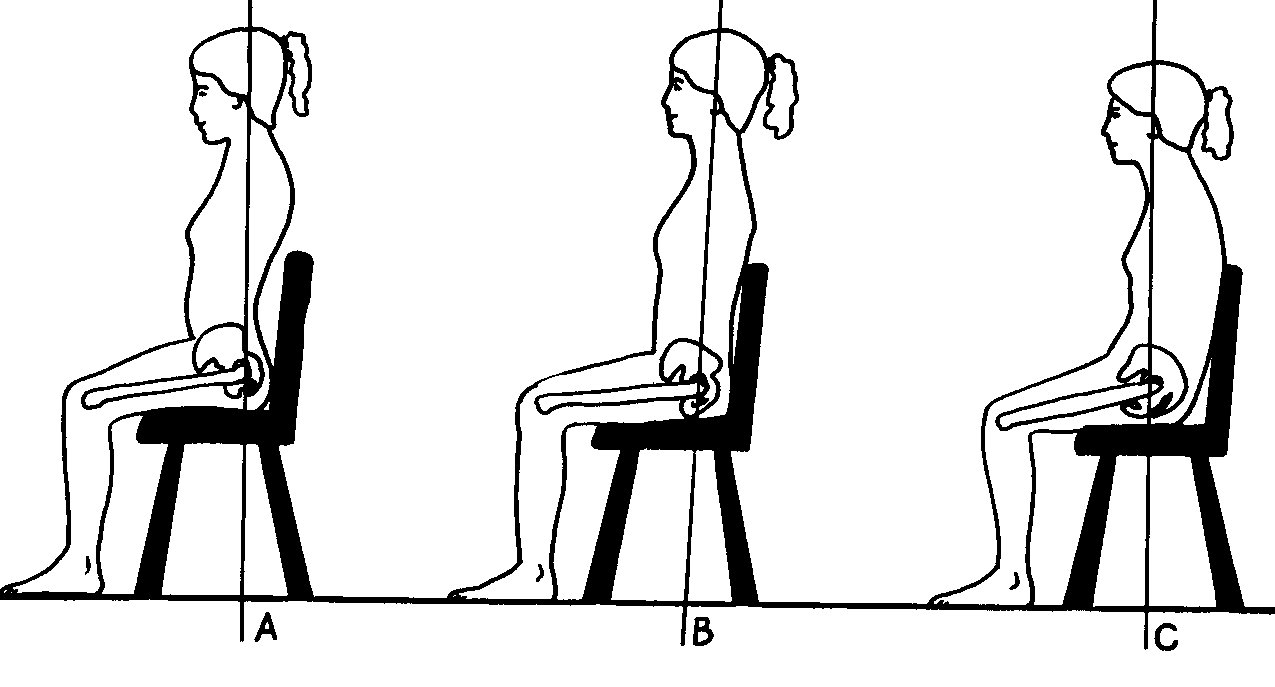
Pelvic floor pain when sitting can be a challenging and uncomfortable condition. It may be caused by various factors, and it's important to identify the underlying cause to determine the most appropriate treatment. Here are some common causes of pelvic floor pain when sitting and potential ways to address them:
Muscle Tension and Overactivity: Pelvic floor muscles can become tense or overactive, leading to pain when sitting. A specific muscle spasm of the rectum is often known as proctalgia fugax. Pelvic floor physical therapy can be beneficial in this case. A trained therapist can guide you through exercises to relax and strengthen these muscles appropriately.
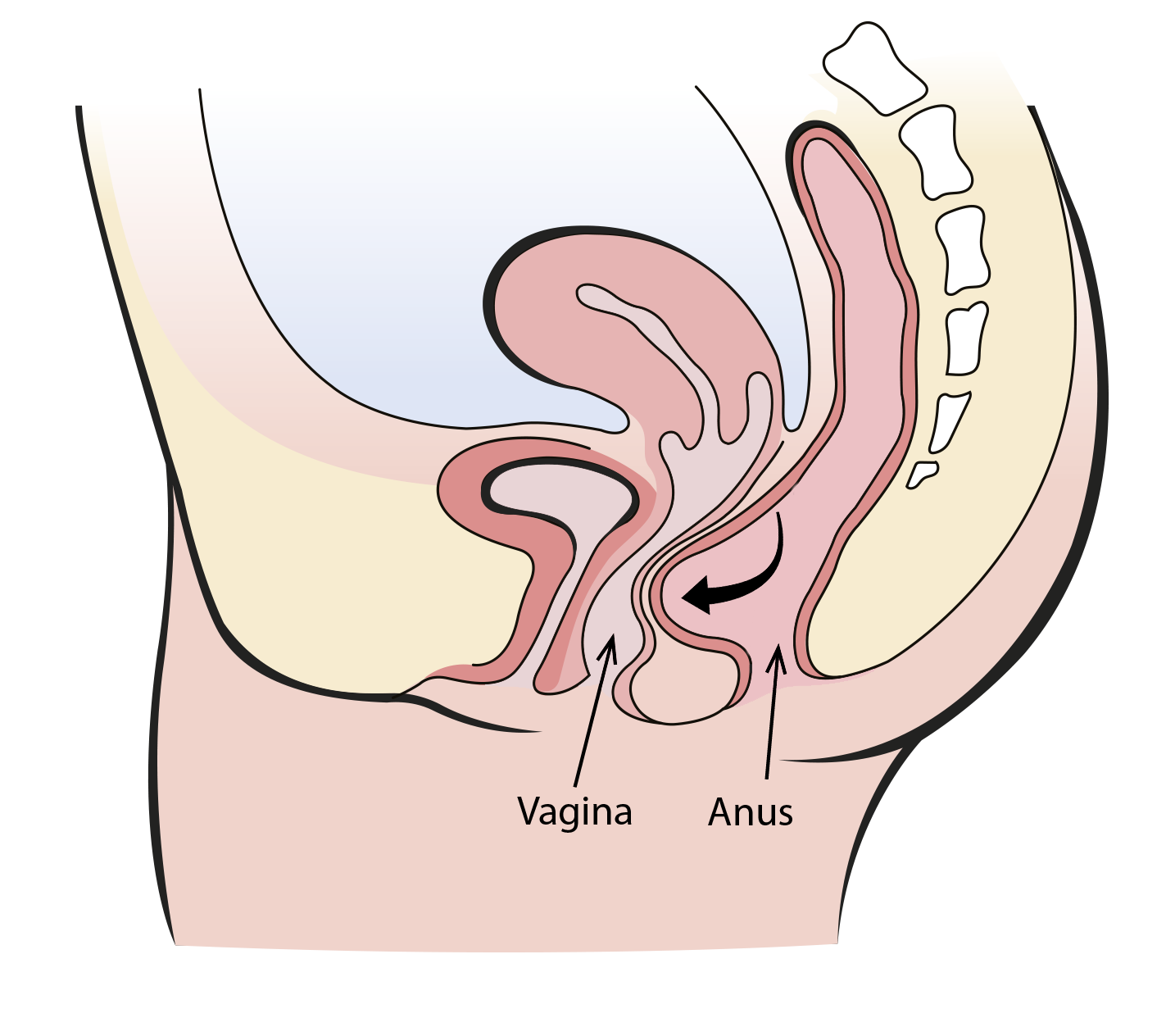
Pelvic Floor Muscle Weakness: Weak pelvic floor muscles can also contribute to pain when sitting. Pelvic floor weakness can lead to pelvic prolapse such as a rectocele, which is a bulge of the front wall of the rectum into the vagina, or a cystocele, which is a prolapse of the bladder. Pelvic Floor Physical therapy can help you strengthen these muscles, improving their support and function.
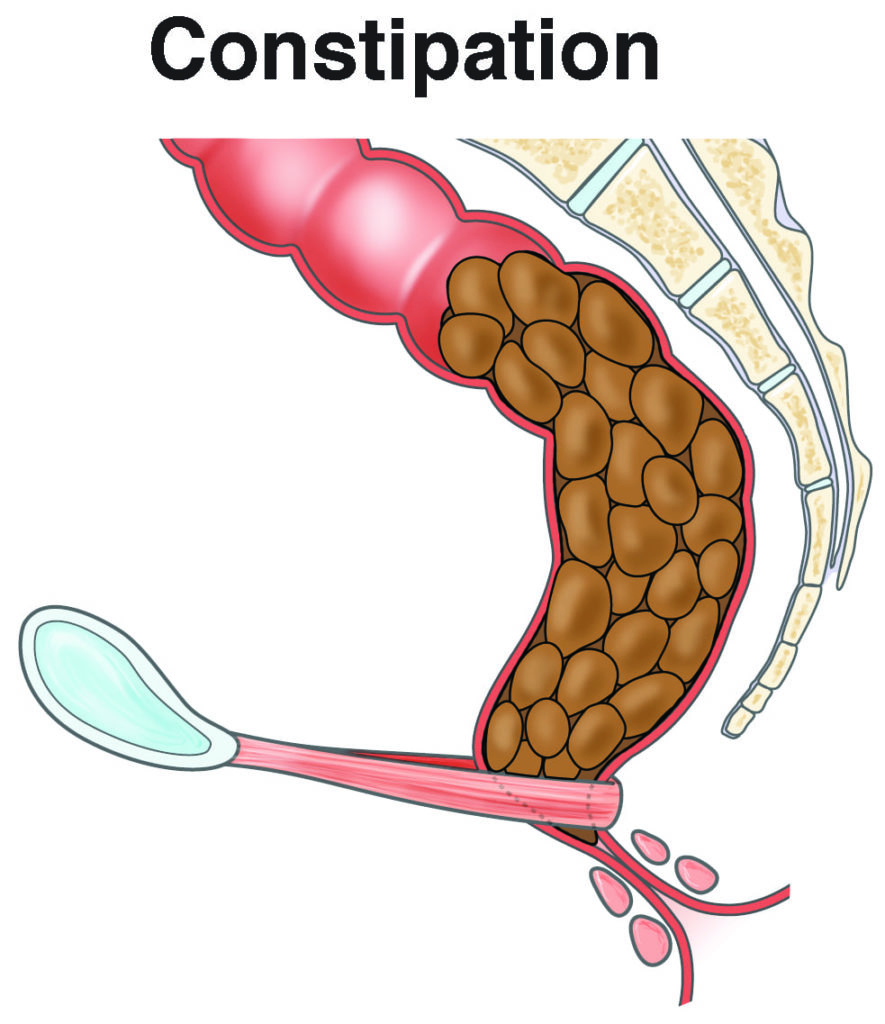
Constipation: Constipation can cause difficulty or obstructions, making bowel movements difficult. When the stool reaches the end of the colon, it can be difficult to empty causing feelings of incomplete evacuation or increased frequency. Straining or the physical stool itself can cause pelvic floor pain with sitting.
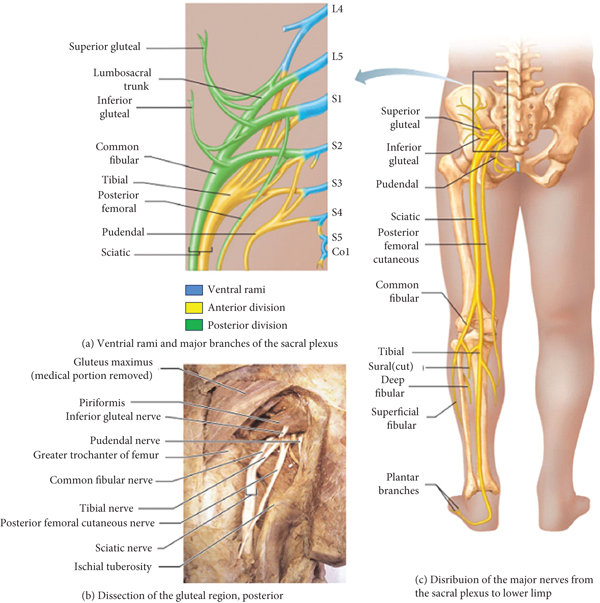
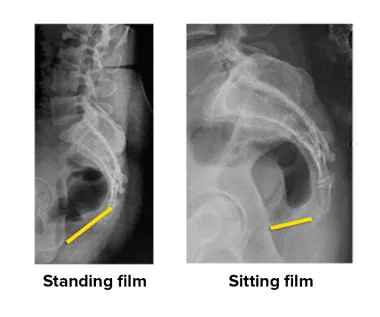
Nerve Irritation: Nerves in the pelvic area can become irritated due to various reasons, such as injury, inflammation, or pressure. The pudendal nerve, sciatic nerve, and posterior femoral cutaneous nerve all exit posteriorly from the sacrum and in a seated position can be entrapped or irritated even more. Treating the underlying cause of nerve irritation and managing pain with medications or nerve blocks may be necessary.
Pelvic Floor Dysfunction: This is a broad term that encompasses various issues related to the pelvic floor, including muscle dysfunction, coordination problems, and pelvic organ prolapse. Treatment may involve a combination of physical therapy, medication, and, in some cases, surgical interventions.
Coccygodynia is pain of the coccyx bone, also known as your tailbone, possibly from a fall or injury. Coccygodynia can cause pain with bowel movements, pain with sitting, or pain with movements. A pelvic floor specialist can check the alignment of your tailbone, the muscles and ligaments attached to the coccyx, and also check to see if there is any scar tissue creating increased tension on the tailbone.
Endometriosis or Interstitial Cystitis: These conditions can cause pelvic pain that worsens with sitting. Consultation with a gynecologist or urologist can help diagnose and manage these conditions with appropriate medications and treatments.
Injuries: Pelvic injuries, such as trauma from accidents or falls, can lead to pain while sitting. Treatment may involve rest, pain management, and rehabilitation therapy.
Infections: Infections in the pelvic area, such as urinary tract infections or pelvic inflammatory disease, can cause discomfort when sitting. Appropriate antibiotics and medical treatment are essential to address these infections.
Hernias: Inguinal or femoral hernias can sometimes cause pelvic pain when sitting. Surgical intervention may be required to repair the hernia.
Inflammatory Conditions: Inflammatory conditions like pelvic inflammatory disease (PID) or irritable bowel syndrome (IBS) can lead to pelvic pain. Treating the underlying inflammation and managing symptoms with medication and dietary changes can be helpful.
If you're experiencing pelvic floor pain when sitting, it's crucial to consult a healthcare provider or specialist who can perform a thorough evaluation, including a physical examination and potentially imaging or diagnostic tests. Based on the diagnosis, they can recommend the appropriate treatment plan, which may include physical therapy, medication, lifestyle modifications, or surgery, depending on the underlying cause of your pain. Remember that early intervention and proper management can help alleviate or even resolve pelvic floor pain.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment