Back
Why Can't I Poop? (Constipation)
By Shannon Strauch, PTA, STMT-1 on 7/3/2024
There are several reasons why someone might have difficulty with bowel movements:
Dietary Factors:
Not consuming enough fiber or fluids can lead to constipation.Lifestyle Habits:
Lack of physical activity or ignoring the urge to go can contribute.Medical Conditions:
Conditions like irritable bowel syndrome (IBS), hypothyroidism, or neurological issues can affect bowel movements.Medications:
Some medications can cause constipation as a side effect.Emotional Factors:
Stress or anxiety can affect bowel function.
Pelvic floor dysfunction can play a significant role in causing constipation and difficulty with bowel movements. Here's how:
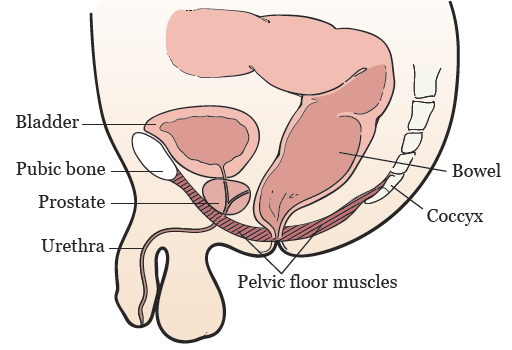
Pelvic Floor Muscle Coordination:
The pelvic floor muscles need to relax to allow stool to pass. If these muscles are not coordinating properly or are too tight, it can make bowel movements difficult.Pelvic Organ Prolapse:
In some cases, organs like the rectum may prolapse or shift out of place, making it harder to have a bowel movement.Dyssynergic Defecation:
This condition occurs when there is a lack of coordination between the pelvic floor muscles and the abdominal muscles, making it difficult to pass stool.Pelvic Floor Tension:
High levels of tension in the pelvic floor muscles can obstruct the rectal passage, leading to constipation.Connective Tissue Differences:
Hypermobility is often related to differences in connective tissue, which can affect the structure and function of the gastrointestinal tract, leading to constipation.
Pelvic floor therapy can be very effective in treating constipation by addressing the mechanics of the pelvic floor and surrounding structures. Here’s how it works:
Mechanics of Pelvic Floor Therapy for Constipation
Pelvic Floor Muscle Relaxation:
Muscle Tension:
When the pelvic floor muscles, including the puborectalis, are too tight or have poor coordination, they can obstruct the rectum and make it difficult to pass stool. Pelvic floor therapy focuses on teaching these muscles to relax properly during bowel movements.
Techniques:
Therapists use biofeedback, manual therapy, and specific exercises to help patients learn to relax these muscles.
Improving the Puborectalis Angle:
Puborectalis Muscle:
This muscle forms a sling around the rectum and helps maintain continence by creating a bend in the rectum. During a bowel movement, the puborectalis muscle needs to relax to straighten this angle and allow stool to pass.
Therapy Focus:
Pelvic floor therapy includes techniques to improve the coordination and relaxation of the puborectalis muscle, making it easier for the rectum to straighten and for stool to pass more freely.

Belly Breathing and Abdominal Muscle Coordination:
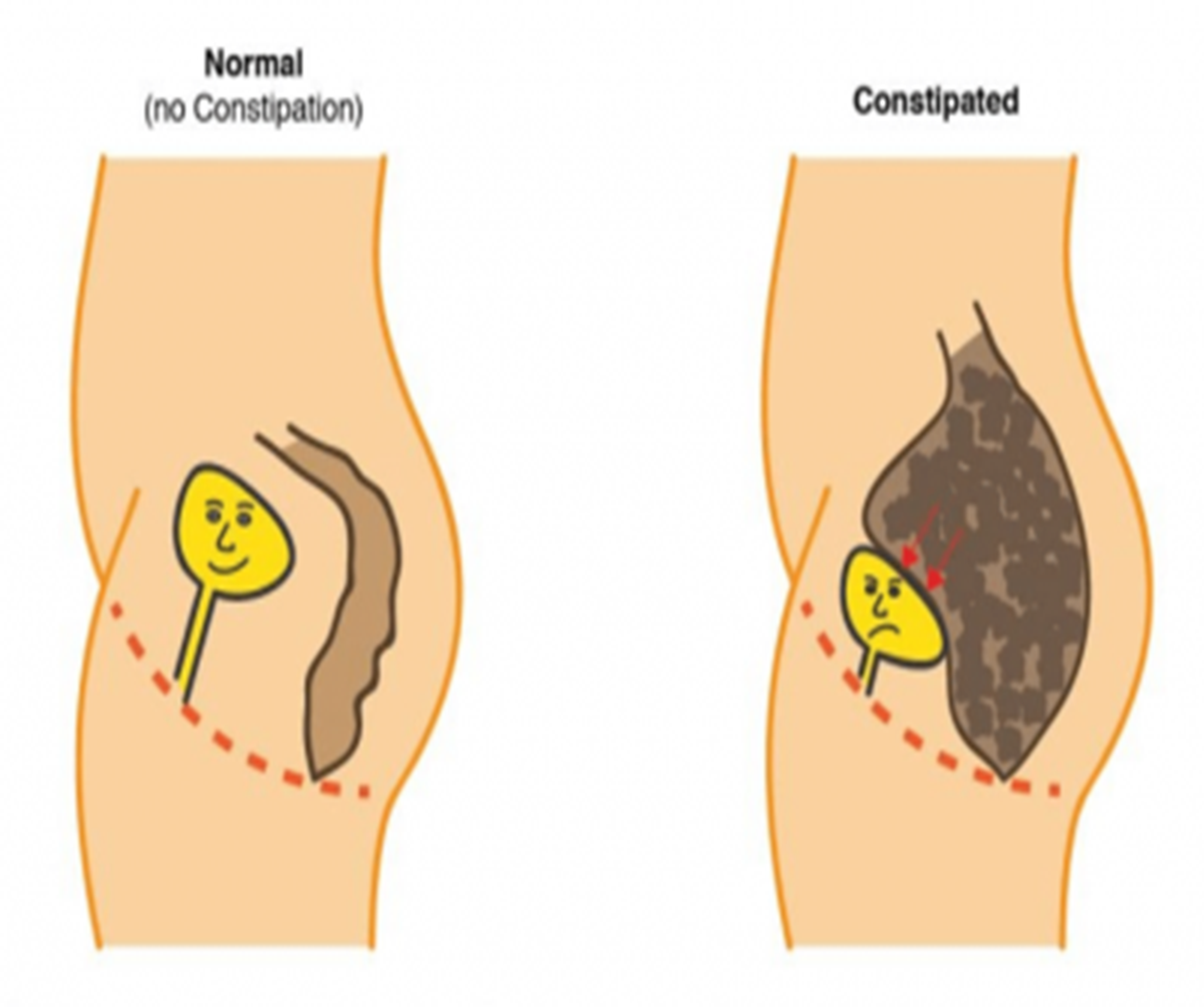
Big, Hard Belly:
Constipation often causes a distended, hard abdomen due to the buildup of stool and gas. Learning proper belly breathing techniques can help manage intra-abdominal pressure and improve bowel movements. Therapists can also teach you how to do a proper self mobilization, or "I L U" massage to help move stool along
Diaphragmatic Breathing:
Therapists teach diaphragmatic breathing, which involves deep, abdominal breathing to help relax the pelvic floor and abdominal muscles. This can reduce the straining that often accompanies constipation.
Postural Adjustments and Pelvic Tilts:
Optimal Positioning:
Pelvic floor therapists may teach patients how to use positions like squatting or using a footstool while sitting on the toilet. These positions can help straighten the anorectal angle and make bowel movements easier.
Pelvic Tilts:
Exercises to improve pelvic alignment and tilts can also aid in achieving a more functional defecation posture.
Strengthening:
Stabilization Exercises:
Pelvic floor therapy can provide exercises to strengthen and stabilize the pelvic floor and surrounding muscles in order to be able to physically push out the poop.
Connective Tissue Support:
Techniques to support connective tissue health and function can also be included in the therapy regimen.
Combined Approach
Combining pelvic floor therapy with dietary changes (such as increasing fiber and fluid intake), regular physical activity, and behavioral modifications (like not ignoring the urge to go) provides a comprehensive approach to managing and alleviating constipation.
By addressing the mechanics of muscle function, coordination, and proper positioning, pelvic floor therapy can significantly improve bowel movements and reduce the discomfort and complications associated with constipation. Looking to optimize your bowel movements with pelvic floor physical therapy? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Chronic Pelvic Congestion in Men Contributes to Prostatitis By Shannon Strauch, PTA, STMT-1 on 12/11/2024 How lymphatic issues can cause symptoms of prostatitis Prostatitis and Tight Pelvic Floor Muscles: A Comprehensive Guide By Shannon Strauch, PTA, STMT-1 on 12/10/2024 How a tight pelvic floor can be the reason for prostatitis symptoms
Are you ready to live pain free?
Request An Appointment